Our Blogs
Visually Access To Your Doctor.
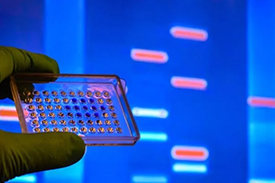
The Future of Personalized Medicine and its Ethical Implications.
The Future of Personalized Medicine and its Ethical Implications. • 14 Feb,2024
Introduction:
Personalized medicine, propelled by advancements in genomics, data analytics, and medical technology, holds the promise of revolutionizing healthcare delivery by tailoring treatments and interventions to individual characteristics. While offering unprecedented opportunities to improve patient outcomes, personalized medicine also presents complex ethical considerations that necessitate careful examination and guidance. This article explores the evolving landscape of personalized medicine and delves into its ethical implications, highlighting key considerations for healthcare stakeholders and policymakers.
1. Genomic Revolution and Informed Consent:
The integration of genomic data into clinical practice raises ethical concerns regarding patient autonomy, privacy, and consent.
Informed consent processes must empower patients to make informed decisions about genetic testing, treatment options, and data sharing while respecting their autonomy and privacy rights.
2. Equity and Access to Personalized Care:
Disparities in access to personalized medicine technologies and treatments may exacerbate existing healthcare inequities.
Ethical frameworks should prioritize equitable access to genetic testing, targeted therapies, and specialized treatments to ensure fair and just healthcare delivery for all individuals, irrespective of socioeconomic status or geographic location.
3. Data Privacy and Security:
Personalized medicine relies on the collection, storage, and analysis of vast amounts of sensitive patient data, raising concerns about privacy breaches and data security.
Striking a balance between data sharing for research and protecting patient confidentiality requires robust data encryption, adherence to regulatory standards, and transparent data-sharing practices.
4. Ethical Use of Genetic Information:
The ethical use of genetic information entails safeguarding against genetic discrimination, stigmatization, and potential psychosocial impacts.
Policies and guidelines should be established to prevent the misuse of genetic data, protect individuals' privacy rights, and mitigate the risks of discrimination based on genetic predispositions or susceptibilities.
5. Clinical Decision-Making and Patient-Centered Care:
Ethical clinical practice in personalized medicine requires transparent communication, shared decision-making, and consideration of patient values and preferences.
Healthcare professionals must navigate complex ethical dilemmas, such as interpreting genetic test results, managing uncertainty, and respecting patient autonomy, to ensure patient-centered care delivery.
6. Research Ethics and Informed Consent:
Ethical considerations in personalized medicine research include obtaining informed consent, protecting participant privacy, and ensuring responsible data use.
Researchers must adhere to rigorous ethical standards, uphold principles of integrity and transparency, and prioritize the welfare and autonomy of research participants.
Conclusion:
As personalized medicine continues to advance, addressing its ethical implications is paramount to promoting patient welfare, protecting privacy rights, and fostering equitable access to healthcare.
